Gordon College at the Forefront: Craig Story Conducts Cancer Research with Immunofluorescence Microscopy
Why do some people get cancer, while others don’t? Our immune system normally identifies and kills bad cells and tumors, so why do some cancerous cells escape? In the race to find cures and answers, cancer researchers need all the help they can get. This often requires specialized equipment, including microscopes and image analysis technology.
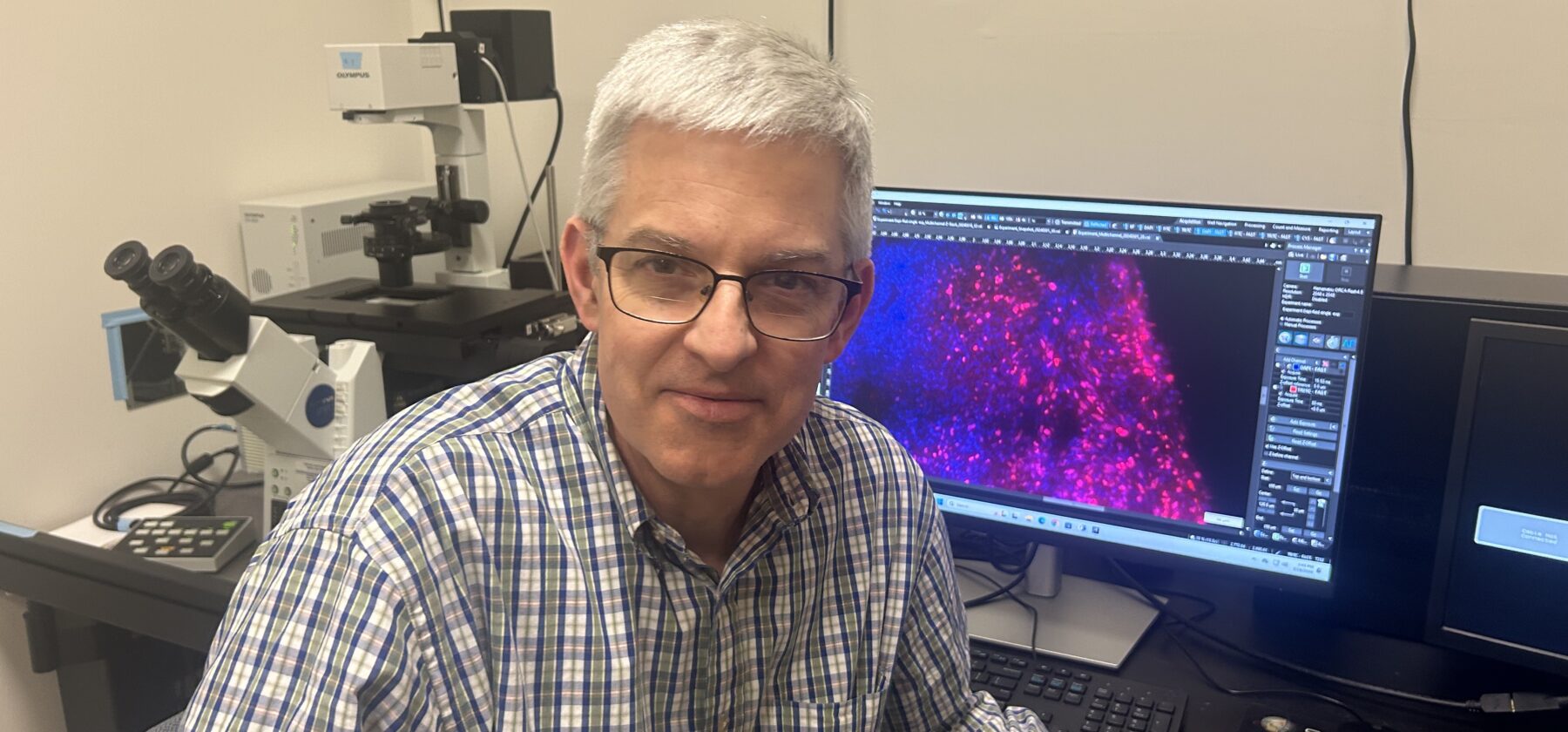
Soon, Gordon College students will be able to help in the quest for cancer answers by doing immunofluorescence microscopy work—a staining process to analyze the state of cancerous cells by creating images of different tumor-associated proteins in the tissue. Gordon’s lab will be counted among the labs in the Boston area that can perform immunofluorescence microscopy, alongside institutions like Massachusetts General Hospital and Harvard, because of the work Dr. Craig Story, professor of biology, began over his sabbatical last semester.
Facts About Pancreatic Cancer: Why Research Matters
Throughout the fall 2023 semester, Story collaborated with Dr. Stephanie Dougan, a principal investigator at the Dougan Lab of the Dana-Farber Cancer Institute, on pancreatic cancer research. Notoriously challenging to treat, pancreatic cancer’s nature and location makes it harder to spot before it reaches Stage IV and metastasizes, according to the National Institutes of Health. Chemotherapy may provide a small benefit, but most efforts to improve on the current regimens consistently and stubbornly fail in advanced clinical trials. The five-year survival rate for pancreatic cancer—the percentage of all patients who are living five years after diagnosis—is very low at just five to ten percent, reports Johns Hopkins Medicine.
In the Dougan Lab researchers study the tumors of mice to understand as much as possible about pancreatic cancer, especially about how tumors behave in mice with slight genetic differences. “If we can figure out why these different kinds of mice have more metastases or fewer metastases, that could provide us information that could be valuable to human therapy,” Story says. “We’re figuring out ways to study the immune response against tumors.”
The Scope of Immunofluorescence Research
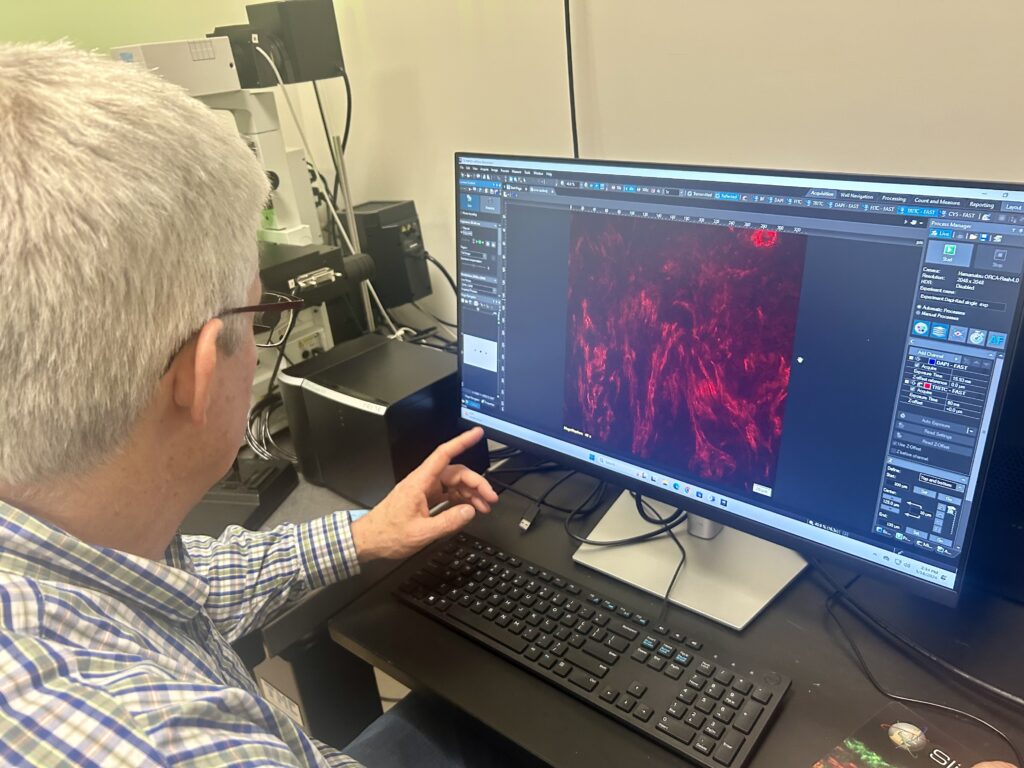
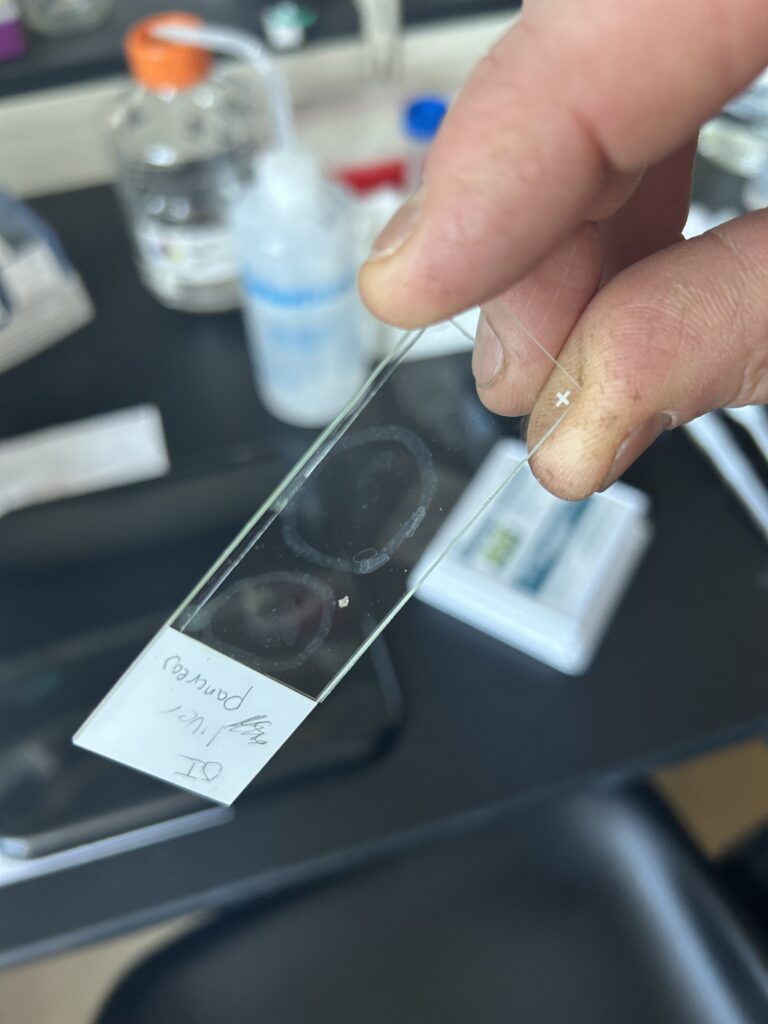
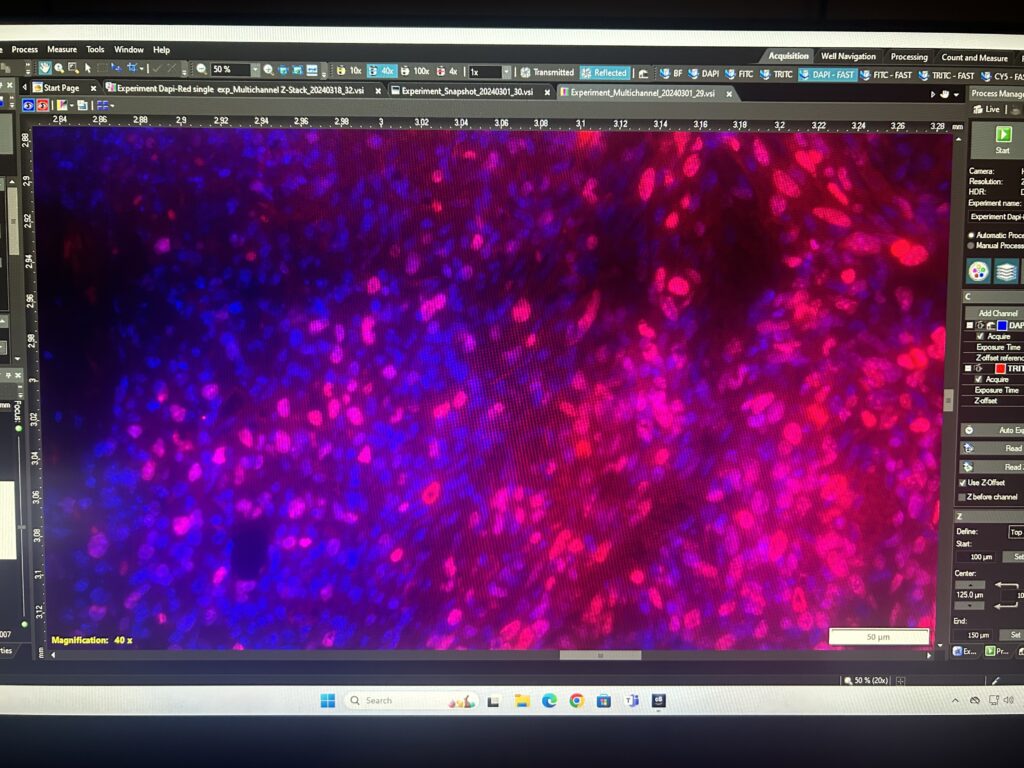
In their research the Dougan Lab grew mice tumors, which were then frozen and given to Story once they progressed enough. With a cryostat Story made tiny slices of the tumor—approximately 10 micrometers (0.01 of a millimeter) thick. Story then soaked the tissue sections with antibodies that have chemically linked fluorescent tags. With the ultraviolet illumination provided by the microscope, the antibodies start to glow neon colors in distinctive patterns based on which antibodies are used, illuminating every cell and protein on the slide. This immunofluorescence allows Story and other researchers to compare the pattern of staining under different conditions. Watching how the tumors behave differently in different mice can be directly visualized and quantified for research.
To see these tiny antibodies, Story used two different microscopes purchased through a Massachusetts Life Sciences Center grant to take pictures of the slides: A standard fluorescence microscope and a laser scanning confocal microscope that uses a laser to create sharp, vibrant, colorful images that reveal specific proteins and cells in the tumor and surrounding tissue. “These microscopes are the same kind as used in top research labs and are mind-bogglingly expensive, so having access to that grant money was a real boon to the college,” Story said.
Dr. Megan “Meggie” Hoffman is the senior postdoc in Dougan’s lab who grew the tumors in the mice and provided the tumor samples. She also helped Story learn and implement the latest methods and software for doing image analysis. Story also upgraded the lab computers to accommodate these required software updates. By watching the patterns of staining of certain antibodies, researchers can understand why certain immune cells respond or fail to respond to cancer cells. If there’s a certain protein involved causing harm or preventing it, they can potentially block or enhance its function as part of treatment.
“The reason why I wanted to pursue this as a project was because it’s the kind of thing that undergraduate students can learn how to do and do very well,” says Story. “My biggest goal is to have students learn how to do this.”
Gordon Joins the Mission
Given the great demand for help in cancer research, Gordon students may soon have plenty of opportunities to help with staining and immunofluorescent work for organizations across Massachusetts and beyond. Immunofluorescence microscopy is a valuable skill that is in demand in many university and industry labs. Students can participate in a key part of important research projects, doing the staining for many types of cancers and other diseases.
“If a certain lab, say in an industry lab in the Boston area, needs to get some tissue staining done or some analysis of tissues, we can take those tissue samples, section them, stain them and do the image analysis, and report to them the results. The more people that we can train in these methods, the faster we can find answers and move farther along the road to curing disease,” says Story.
Pictured above: Dr. Craig Story with a standard fluorescence microscope to the left and an image of a stained mouse tumor slice on the computer to the right.
 The Bell
The Bell